
Knee Osteoarthritis
Mar 23, 2016 by Adam Bernard MSc.PT, CG-IMS
In the last blog we discussed the difference between osteoarthritis (OA) and rheumatoid arthritis (RA). Today we will look at a joint that is often affected by OA. The knee. The knee is made up of 3 major bones: the femur (thigh bone), the tibia (shin bone) and the patella (knee cap). 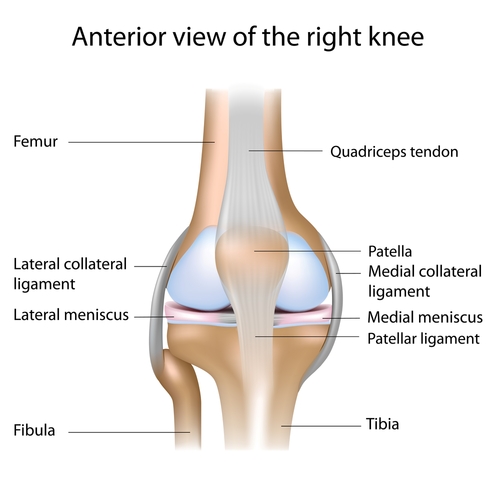
As we discussed in the last blog, OA is a progressive pattern of traumatic and age dependent degenerative changes. This results in a loss of articular cartilage (meniscus) and a subsequent reactive bone formation. These changes may lead to functional changes including difficulty rising from a chair, standing, walking, and stairs among other activities of daily living.
There are 5 main stages of knee OA. These include:
- Breakdown of articular cartilage - The cartilage breaks down, the bones at the joint become rough, and the joint space begins to narrow.
- Synovial irritation – The joint becomes inflamed or irritated.
- Remodelling – The bone begins to increase in density and osteophytes (small bone growths) begin to form in the area.
- Eburnation of bone – The bone becomes more exposed. This is a painful stage and micro fractures can occur leading to increased bone density.
- Disorganization – The joint becomes stiff and unstable. As the joint space narrows, the ligaments that were once taut now become loose and unstable potentially leading to further injury.
Knee OA can develop from physically demanding occupations (jobs that require increased squatting or kneeling), obesity, or previous injury (example: torn meniscus or ligament). Some of the signs of knee OA include: Stiffness (especially in the morning or after rest), swelling (minimal – severe), warm to touch, pain with weight bearing and sometimes at rest, decreased knee range of motion, muscle weakness, and atrophy (breakdown) especially in the quad muscles. The medial or inside part of the knee is most often affected.
Physiotherapy can play a role in treatment. Treatment may include: Manual Therapy, thermal modalities (Eg. Ultrasound), IMS, and Exercise such as strengthening the quads and stretching the hamstrings. Treatments such as: NSAID’s (anti-inflammatories), cortisone injections, weight loss, and proper footwear can be beneficial. In some cases surgery may be required.
